Michael Joe Cini
29th March 2023
Smartphone Technology Takes On Anaemia Detection
Researchers at the University College London and the University of Ghana have touched upon a breakthrough for quick and inexpensive haemoglobin testing. Their new smartphone-based system is designed to use phone cameras to detect haemoglobin concentrations, offering a new way for medical staff to detect anaemia.
Turning a smartphone into a medical device – How it happened
Noting the importance of devising an inexpensive, reliable way of testing haemoglobin levels, researchers at the two institutions turned to a device used worldwide – smartphones. The real hurdle was figuring out how to turn a smartphone into a diagnostic tool that could be relied upon. As one of the leads of the project, Thomas Wemyss of the University College London, said, “Smartphones are globally popular, but research using smartphone imaging to diagnose diseases shows a general trend of experiencing difficulty when transferring results to different groups of people.”
Their study was not the first one revealing how researchers are examining the prospects of using a smartphone as a tool for medical examinations, though. For example, a team at Purdue University recently published a study detailing the use of smartphones to detect haemoglobin levels by taking pictures of the inner eyelid. Even earlier in 2014, a University of Washington team developed an app to detect neonatal jaundice using only a smartphone camera and a tiny colour calibration card.
The team, which had experienced prior success in screening for neonatal jaundice using smartphone-based technology, began work in 2018. Principal investigator Dr Terence Leung, an Associate Professor in Biomedical Optics at University College London’s Department of Medical Physics and Biomedical Engineering, commented in a press release, “we are so excited to see that the smartphone imaging technique can also apply to anaemia screening in young children and infants.”
The technology works by taking images of body parts with little pigmentation, such as the sclera (white) of the eye, lower eyelid, and lip. The app then analyses the colour of the imaged tissue using absorbance analysis techniques. Haemoglobin absorbs light in a specific fashion, and the app can analyse the light from the photographs to determine haemoglobin concentrations. After adjusting for varying ambient lighting and chromaticity metrics for the region captured, the app can give a fairly accurate result.
Promising results from smartphone Colourimetry
The findings from their pilot study were published in the March 2023 issue of the journal PLOS ONE and outlined how their algorithm could test for haemoglobin levels. The researchers recruited sixty-two patients under four years of age at Korle Bu Teaching Hospital, Ghana. After testing, highly promising results were obtained; the app had a sensitivity score of 92.9% and a specificity of 89.7%.
As the researchers wrote, the evidence suggested, “smartphone colourimetry is likely to be a useful tool for making anaemia screening more widely available.” Will it replace the currently-used analysers? Not yet, it seems. The researchers still have to determine optimal methods for image pre-processing, particularly across diverse populations, and it will need to receive wide adoption across multiple countries. However, it offers the promise of reliable, non-invasive, and affordable testing for a disease with a significant burden. With more clinical trials, it may be set for adoption in low- and middle-income countries soon.
Anaemia: A major burden in the human population
Blood haemoglobin concentration is one of the most reliable measures for detecting the presence or absence of anaemia. However, access to the equipment used to measure haemoglobin concentrations is not equally distributed worldwide, with the effect pronounced in low- and middle-income countries with unequal access to routine medical diagnostics.
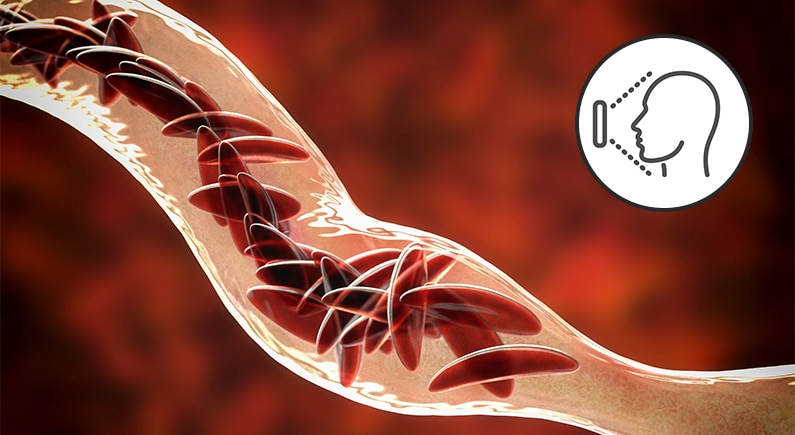
One of the essential components of blood is the red blood cell, which makes up about 45% of blood in most healthy people. The red blood cell’s chief function is to carry Oxygen, which the body’s tissues and muscles require to generate energy. Red blood cells, also known as erythrocytes, carry Oxygen by binding it to a molecule known as haemoglobin. When the red blood cell arrives at tissues lacking Oxygen, it releases its Oxygen payload.
In certain individuals, however, the number of red blood cells present in their blood is insufficient to supply all the body’s cells with Oxygen. This condition is known as anaemia. It is one of the most common diseases globally, affecting over two billion people, particularly in low-income countries. Characterized by symptoms such as fatigue, weakness, heart palpitations, pale/yellowish skin, and dizziness, anaemia can develop due to various causes. Children, especially new-borns, have more at stake in a case of anaemia: the condition can negatively affect cognitive development and lead to increased disease susceptibility.
Access to testing – A problem in low-income countries
Usually, anaemia occurs due to iron deficiency – about half the cases, according to an article in the Lancet. Therefore, it is readily treatable by iron supplements if it is detected. In high-income countries, haemoglobin levels are routinely tested in medical check-ups. In low- and middle-income countries, this is often not the case. Firstly, laboratory procedures can be relatively expensive, and access to a clinic may not be easy to come by for most residents of these countries. The distance to hospitals is often long. Families typically have to make at least two trips – one for sample collection and another for receiving results.
What about automated analysers such as blood analysers and automated haematology analysers? While such devices are readily available from manufacturers, the costs associated with obtaining and using such devices are often too high for local clinics. For one, the initial price for an automated haematology analyzer is high. The cost is further increased due to a need for stable conditions, regular maintenance, and personnel costs to operate the device.
For healthcare workers in low- and middle-income countries, such devices are effectively out of their reach. However, the burden of anaemia in the world is significantly heavier in these regions. The Global Burden of Disease Study in 2019 reveals as much. In a study published in the Journal of Hematology & Oncology, researchers found that the highest national anaemia prevalences were in Zambia, Mali, and Burkina Faso, with Zambia recording as high as 49,000 cases per 100,000 people. All three most-affected regions are located in low-income areas, underlining the need for innovative, accurate, and inexpensive testing to help reduce the disease burden in these countries.
Med-Tech World News for the latest insights on medical technology!
Stay up to date with the latest news and analysis on medical technology, innovation, and healthcare by visiting Med-Tech World News. Our team of experts provides in-depth coverage of the most important topics and trends shaping the industry. Don’t miss out on valuable insights that can help you stay ahead in this fast-paced field.
Start your journey with the Med-Tech World Podcast below!






