Virtual reality will play a pivotal role in patient and doctor medical education
The role of virtual reality (VR) in patient and doctor medical education is going mainstream
Words by Dr. Ryan Grech and Dr. Dylan Attard, Clinical & Health Tech Advisors for MedTech World and two of the co-founders of Digital Health Malta.
In the previous article, Dr. Ryan Grech and Dr. Dylan Attard discussed how the COVID-19 pandemic highlighted the importance of mental health going digital.
If you’re anything like us then when you think of virtual reality (VR) your mind probably wanders to a sandy beach under the tropical sun with a refreshing beverage in your hand. How could you not when we’ve been stuck without travelling for the past year or so! However, VR is so much more than that. We think that VR can change different parts of healthcare delivery for both patients and doctors alike. Although it is not mainstream yet, its popularity is increasing and the advocates for VR are also doing so.
Whilst VR application in healthcare is wide such as rehabilitation, mental health, pain control and much more, we have decided to focus this piece on education as we believe that it is a section where VR can have a significant impact in the short term.
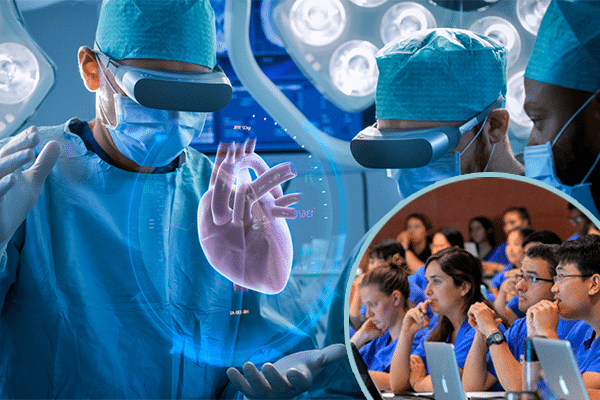
Medical Education
Prof Shafi Ahmed, a colorectal surgeon and entrepreneur, conducted the first VR surgery in 2016. The surgery was viewed by thousands of individuals in multiple countries around the world in real-time (with a 1-minute delay in case of any complications) from the point of view of the surgeon. VR is an excellent tool for teaching. Multiple companies are employing the use of VR to train aspiring surgeons where they can practice operations. The advantages here are a lot; first of all, practice makes perfect – the more a surgeon can repeat a procedure the more proficient he or she will become. VR also allows the young surgeons to look from the point of view of the primary operator enabling them to understand the procedure better. VR is also available 24/7 and in some cases can also be accessed at home and therefore repeated over and over again. We always like to use evidence and a recent study from Harvard Business Review showed that VR-trained surgeons had a 230% boost in their overall performance compared to their traditionally-trained counterparts.
Anatomy teaching has also been revolutionised. Students can now just put on a headset and follow the sacral nerve whilst removing surrounding muscle and bone and rotate the structure by 360 degrees making it easier to understand its path better. We may be entering an age where you do not need to go to a cadaveric dissection session. Anatomy via VR is again accessible on-demand but also offers a superior experience to traditional teaching as allows modification and creation of infinite viewing angles again helping students grasp anatomy better.
Finally, medical schools can create infinite simulations for their students which helps prepare them for the real-life junior doctor environment they are going to be working in. From acute cases to rare cases, dealing with difficult patients or families medical schools can adequately equip their students to deal with the different scenarios which they would otherwise not have encountered in traditional training. We believe that this will make better junior doctors in the long run as you’re inevitably building confidence and testing limits in a controlled and safe environment thus promoting learning.
Patient Education
Anecdotally we have seen that patients who are well informed before surgery tend to fare better. We think this is because they are more in control and know what to expect in different circumstances thereby reducing anxiety levels. Similarly, patients who are more educated about their condition tend to have their illness more under control be it their blood glucose or their cholesterol levels.
We are not saying that the onus rests solely on the patient as we do understand that sometimes it can be difficult to keep up with what doctors say. Admittedly, at times we may not be great communicators.
It’s been shown that following an appointment, patients routinely forget over half of the instructions that their physician gave them. This not only ends up being an issue as it results in increased admissions but in some instances the lack of information retention can be potentially threatening (imagine a patient taking an incorrect dose of blood-thinning medication).
We believe that VR can help explain information in an easy and standardised manner especially for those who are more visual learners. This therefore can close the retention gap. Once again is available on-demand for the patient to see and repeat as they please. Apart from that we also think that VR can accelerate behaviour change, for example, drinking soda which leads to a myriad of complications such as diabetes and obesity. People tend to have a psychological distance with certain risk behaviours such as increased sugar intake likely because they do not perceive it as an imminent threat. However, using VR patients may be shown the consequences of their actions, diabetes, obesity etc. in the hope that the message sticks, hopefully converting their behaviour to a healthy one.
The benefits may extend to the caregivers too, who need to also understand better their loved one’s condition to be able to care for them.
We believe that in the next 3 years, the above will be commonplace. We are already extremely excited by the start-ups in this sphere and are eager to see how it will develop further in the months to come. We can’t wait to use them ourselves, after all, learning is a lifelong process.
See also by the authors: AI in healthcare: “We have an opportunity to finally have true health equality”